Is MDMA Neurotoxic?
Is MDMA Neurotoxic?
And if so, what does that mean?
There have been a lot of press reports (and even anti-drug ad campaigns) about the neurotoxicity of ecstasy. Magazines and newspapers have printed frightening stories suggesting that even a single dose of ecstasy can cause permanent brain damage. It’s been claimed that ecstasy use may eventually lead to disorders ranging from depression to Parkinson’s disease. Finding the truth about MDMA neurotoxicity amidst all these rumors can be difficult. It can also cause anxiety. You may become panicked, interpreting every change in your mood or mental state as evidence of brain damage. Or, you may be inclined to dismiss all claims of MDMA neurotoxicity because so much of what you see in the popular press is clearly exaggerated.
We’ve tried to avoid both these extremes and present only well documented and factual information in an unbiased and useful way. (Our MDMA Neurochemistry Slideshow can help you to understand some of the brain anatomy discussed here.)
Contents
What is MDMA Neurotoxicity?
What causes MDMA (‘ecstasy’) neurotoxicity?
Can we check people for neurotoxicity?
Do ecstasy user’s brains show signs of neurotoxicity?
How large of a dose would be neurotoxic in humans?
What can I do to make sure I don’t get neurotoxic damage from MDMA?
Does Prozac prevent MDMA neurotoxicity?
How would MDMA neurotoxicity affect you? Do I have neurotoxicity?!?
Does MDMA cause Parkinson’s?
Does MDMA make holes in your brain?
What is MDMA Neurotoxicity?
 In laboratory animals, large or frequent doses of MDMA can destroy serotonin axons. Serotonin neurons (brain cells) form a sort of control system in your brain, regulating emotions, appetite, sleep and other functions. The serotonin axons are ‘communication cables’ that the serotonin system uses to send its signals to the rest of the brain. (MDMA works primarily by causing these serotonin axons to release a lot of serotonin at once, causing euphoria.)
In laboratory animals, large or frequent doses of MDMA can destroy serotonin axons. Serotonin neurons (brain cells) form a sort of control system in your brain, regulating emotions, appetite, sleep and other functions. The serotonin axons are ‘communication cables’ that the serotonin system uses to send its signals to the rest of the brain. (MDMA works primarily by causing these serotonin axons to release a lot of serotonin at once, causing euphoria.)
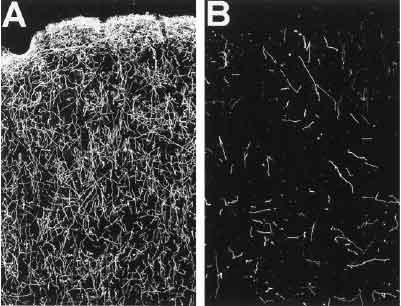
These two pictures show slices of a monkey’s brain. The serotonin axons have been stained to make them appear as bright lines. The picture on the left (A) is from a normal monkey. The picture on the right (B) is from a monkey that was injected with a very large dose of MDMA.1 As you can see, many of its serotonin axons have been lost. (Animal research suggests that when a neurotoxic dosage of MDMA is given, damage to the axons starts to occur in as little as an hour or two.) Animal experiments suggest that if neurotoxicity occurs, some new serotonin axons can grow to replace them…but they grow in different places than where the original ones were.[2] The long-term effects of this ‘rewiring’ are not known.
What causes MDMA neurotoxicity?
Scientists aren’t sure yet. What we do know is that some chemical gets into the serotonin axons through the SERotonin Transporters (SERTs), tiny molecular pumps that neurons use to collect serotonin. (Visit the Ecstasy Slide Show for more information.) Once inside, this chemical is broken down by an enzyme.[7] This breakdown process creates oxidizing chemicals (like hydrogen peroxide) that can damage the neuron. We aren’t sure what that first mystery chemical is. For a long time, we thought it was probably dopamine, which we knew played a role in neurotoxicity (dopamine is another neurotransmitter, like serotonin, that is released by MDMA.) However, more recent research has discovered that dopamine’s main role in promoting MDMA neurotoxicity is by increasing body temperature: significant overheating is a very important factor in whether or not MDMA neurotoxicity will occur.[8]
As far as what the actual toxic chemical might be, there are several theories. The most popular theory is that a hepatic metabolite of MDMA (a broken down form of MDMA created in the liver) is to blame.[9] Another theory suggests that MDMA itself may be the ‘toxic chemical’, since there is evidence that MDMA itself may be broken down in the brain.[10]
Can we check people for neurotoxicity?
It’s difficult to identify and count serotonin axons in brains (even when you can remove and slice the brain up, as was done in the above image) so scientists estimate the numbers and locations of these axons by scanning for markers…substances that are found mainly on serotonin axons. The most useful method for examining human user’s brains looks at the SERT proteins. Because SERTs are found in large numbers on serotonin axons, if somebody loses serotonin axons, the number of SERT proteins detected should also be lower than normal. In order to count SERTs, researchers can give the person or animal a tracer…a chemical that sticks specifically to the SERT and shows up on a brain scan. Then, when the scan it taken, the researchers can see how much of the tracer has temporarily ‘stuck’ in different parts of the brain. If a lot of serotonin axons have been destroyed in an area of the brain, then there won’t be anything for the tracer to stick to, leaving a ‘dark’ region of the brain. 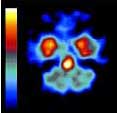 3
3
This graphic shows a PET scan of a human brain, using a tracer that ‘sticks’ to SERT proteins. The brighter colors are areas with more SERTs (and thus, presumably, more serotonin axons.) This is a healthy, normal brain; the dark areas are simply parts of the brain where there are naturally relatively few SERTs (the distribution of serotonin axons isn’t even throughout the brain.) Brain scans can’t normally ‘see’ the serotonin system; it only becomes visible to the scanner when a special tracer is used. (So if you have a brain scan for some other reason, there’s no way for it to detect whether or not there is damage to your serotonin system.)
Do ecstasy user’s brains show signs of neurotoxicity?
This has proven to be a surprisingly difficult question to answer. People who have recently (within several weeks) used ecstasy do usually have fewer detectible SERT proteins, which suggests that axons could have been lost. However, former users who have been abstinent for some time (months to a year or so) seem to have normal levels of SERT, as seen in these results from a large German study looking at the brains of people who had used approximately 800 tablets (on average) of ‘ecstasy’ over their lives:
As you can see, there were small reductions in the number of SERTs detected. However, these changes went away after the ‘ecstasy’ users had stopped using drugs for a few months.
Researchers aren’t absolutely sure what these results mean. Some people think this ‘recovery’ could be the result of surviving axons growing or changing (producing more SERTs) to compensate for destroyed axons. Others argue that the short-term reduction in SERT density might not have been due to lost axons, but could be the result of the neurons simply changing the number of SERTs in response to drug exposure. (A number of prescription drugs that affect serotonin but do not damage neurons also cause a reduction in SERT.[5])
It’s not known what practical effect, if any, these changes might have had on these ecstasy users; a follow up study found that their mental health was poorer than that of non-drug users, but no worse than that of people who used other drugs (such as marijuana) but not ecstasy.[6]
There is some support for the theory that these are just temporary adaptive changes (a little like sun exposure causing a tan) from animal research. When baboons were repeatedly injected with large doses of MDMA (enough to destroy much of their serotonin system), then allowed to recover for several years, new serotonin axons did grow. However, they grew back in abnormal ways, with much higher than normal levels of axons in some parts of the brain, while other areas remained permanently depleted.[2] Since normal pre-use levels of SERT were restored in the German study, it seems more likely that the changes seen were the result of temporary, reversible changes rather than brain injury.
How large of a dose would be neurotoxic in humans?
Unfortunately, we don’t really know. George Ricaurte, the main US-government funded researcher studying MDMA neurotoxicity, has claimed that even a small recreational dose (1.28 mg/kg) of MDMA could be neurotoxic.[11] Other researchers have given human volunteers moderate doses (1.5 mg/kg, equivalent to about one good pill for a 150 pound person) of MDMA with before-and-after brain scans, and could find no signs of damage.[12] Doses of MDMA that produce neurotoxicity in lab animals have generally been considerably higher than a human user would normally take, but smaller animals are also usually more resistant to drug toxicity than humans.
As a result, just because a given dosage doesn’t appear to cause damage to a rat or monkey’s brain doesn’t necessarily mean that dosage is safe for humans. In 2002, the US government’s Food and Drug Administration (FDA) granted approval for using MDMA on human volunteers at recreational dosage levels, which suggests that the government’s medical experts do not believe there is a significant risk of harm from a few moderate doses of MDMA under controlled circumstances with medical supervision. (For more information on this research, visit MAPS.org.)
Although there is considerable debate over how much MDMA it would take to cause damage to a human user’s brain, there is no real doubt that at some dosages damage can and will occur. Fortunately, brain damage doesn’t seem to happen at moderate recreational doses.
What can I do to make sure I don’t get neurotoxic damage from MDMA?
There is only one absolutely proven, foolproof way to avoid neurotoxicity and other risks: Don’t use drugs. If that’s not an option for you, there are still some things that we believe can reduce the risk of neurotoxicity.
Only take one dose on a given day/weekend. It’s a common practice among ravers to take more ‘ecstasy’ when they start to ‘come down’ off the first dose. While this may keep the party going, it may also be dangerous; the more pills you take in an evening, the greater the risk is of all sorts of bad things happening, including neurotoxicity.
Don’t mix MDMA with other stimulants, such as amphetamines (speed/meth.) Combining other stimulant drugs with MDMA is a bad idea; the combination increases the risk of becoming seriously overheated, which we know is a major risk factor for neurotoxicity (and death and liver damage and many other bad things.)
Be aware of overheating risks and avoid hot environments. It’s much easier for your body to keep itself cool if the air temperature is low. In one experiment, rats placed in a cool room suffered no neurotoxicity from a dose of MDMA that extensively damaged the brains of rats in a warm room.13 If you’re going to be out dancing, pick a club that’s cool and has good air flow, and regularly take short breaks to cool off and assess how you’re doing.
Take antioxidants like vitamin C and vitamin E. Because MDMA neurotoxicity ultimately happens through oxidation, antioxidants may be able to provide some additional safety margin. An appropriate dose may be 2-4 capsules or tablets of each around the same time that you take the ‘ecstasy’ pills. In one mouse experiment, mice fed a severely vitamin E deficient diet suffered severe neurotoxicity from a dose of MDMA that didn’t noticeably harm mice on a normal (plenty of vitamin E) diet.14 Antioxidants aren’t just for ecstasy users, either; alcohol and cigarette users can probably also benefit (although in different ways, such as reducing liver damage from drinking.)
There are no absolute guarantees. While there are things you can do (and avoid doing) to reduce risk (probably by quite a bit), any drug use poses inherent risks.
Does Prozac prevent MDMA neurotoxicity?
SSRIs (prescription anti-depressant drugs, such as Prozac, Paxil and Zoloft) stick to and block the SERTs. Because of this effect, SSRIs can reduce the ability of the chemical that causes MDMA neurotoxicity (whatever it is) to get inside the axon and cause damage.15 However, in doing so they also reduce MDMA’s ability to work. As a result, people who are on daily doses of SSRIs may be safe from neurotoxicity, but they usually don’t feel the normal effects of MDMA either. The idea of using SSRIs to prevent neurotoxicity is something of a catch-22: If you take the SSRI after coming down from the MDMA, it’s probably too late to do a lot of good. On the other hand, taking an SSRI before-hand tends to reduce the desired effects of MDMA, making it more logical to simply take less MDMA in the first place. All things considered, it’s unlikely that taking an SSRI before or after MDMA is a very useful prevention strategy. Since SSRIs have their own side effects and potential risks, the practice should probably be avoided.
How would MDMA neurotoxicity affect you?
It might produce symptoms similar to depression: Sleep and memory problems, anxiety, emotional instability, trouble concentrating, etc.
I used a lot of ecstasy, and now I have symptoms like that! Do I have neurotoxicity?!?
Not necessarily. When conditions in your brain change (such as when you take a drug), your brain will adapt to try to counteract the change. These adaptations are the basis of drug dependence and drug tolerance (most of us are highly tolerant of caffeine because our brains have made themselves less sensitive to it in response to regular exposure.)
Since MDMA works mainly by releasing large amounts of serotonin, your brain tries to adapt to the drug exposure by reducing its sensitivity to serotonin. This is a protective reflex, much like jerking your hand away from a hot pan. After the drug is gone, your brain takes its time returning to normal (after all, something strange happened and your brain wants to stay ready in case it happens again!)
Here’s a graph showing “available serotonin receptor density” (how sensitive the brain is to serotonin) in rats before and after being given a very large dose of MDMA:
 The first bar (control) is the rat’s sensitivity to serotonin before any drugs were given. 0.25 days (8 hours) after being given MDMA, much of its serotonin receptors had been ‘turned off’. Over the next 3-4 weeks, sensitivity slowly returned to normal.[19]
The first bar (control) is the rat’s sensitivity to serotonin before any drugs were given. 0.25 days (8 hours) after being given MDMA, much of its serotonin receptors had been ‘turned off’. Over the next 3-4 weeks, sensitivity slowly returned to normal.[19]
This temporary loss of sensitivity to serotonin would probably cause symptoms similar to actual neurotoxicity. With neurotoxicity, the serotonin signal isn’t being sent as strongly (since some of the axons sending it have been destroyed.) With neuroadaptation, the brain can’t hear the serotonin signal as well (since it has fewer receptors ‘listening’.) The end result is the same: The brain receives fewer signals from the serotonin system.
This phenomenon of neuroadaptation is probably the reason why frequent ecstasy use inevitably catches up with people; if you don’t give your brain enough time to re-adjust before the next dose, that next dose can drive things even further away from normal. Pay close attention to your mental and emotional state if you use ecstasy: If you start to feel a little emotionally fragile or mentally ‘fogged’, take a break from use (at least two or three months, preferably more.) Users who feel ‘e-tarded’ from over-indulgence usually report feeling much better after a period of abstinence.
Does MDMA cause Parkinson’s?
In the fall of 2002, there was a research report from George Ricaurte (the ‘top’ US government MDMA researcher) that claimed that MDMA was capable of damaging the dopamine systems of monkeys (not just the serotonin system) at doses similar to those taken by human users.[20] Since Parkinson’s disease is caused by the death of dopamine neurons, it was suggested that damage to the dopamine system from MDMA might produce symptoms similar to Parkinson’s. A year after it was published, the research was retracted when it was discovered that the animals hadn’t been given MDMA at all! Instead, they had been given massive doses of methamphetamine, a much more toxic drug. Ricaurte further admitted that no matter what they had tried, they were unable to damage the dopamine systems of monkeys with real MDMA. (You can read all about this controversy, its fallout, and media coverage of the scandal at MAPS.)
If the retraction wasn’t enough, there have also been several experiments using PET scans to examine the dopamine systems of human ecstasy users, both of which failed to find even temporary changes.[22],[23] MDMA does not cause Parkinson’s.
Does MDMA make holes in your brain?
Not that we know of. This popular but apparently incorrect idea came from a pair of PET scans shown on the Oprah TV show; one from a normal patient’s brain, and the other from an emotionally troubled girl who had used a number of drugs (including ecstasy.)
This is the normal brain….
…and this is the girl’s brain.As you can see, there are visual ‘holes’ in the girl’s PET scan. However, these don’t represent literal holes in her brain; rather, they are areas where there was relatively low blood flow or sugar consumption (the brain runs primarily on sugar.) It’s a very strange brain scan, but there’s no way to know what caused this effect or whether it’s the result of damage or something temporary (depression, fatigue, and various drugs can alter brain activity.)
MDMA does have some effects on blood flow in your brain, both while you are high and for several weeks afterwards (serotonin receptors affect blood flow.) However, studies of blood flow in user’s brains haven’t found lasting changes.24 When researchers gave human volunteers brain scans to examine blood flow, gave them recreational doses of MDMA, and performed follow-up brain scans for several weeks they found that there was somewhat reduced blood flow in their brains after use, but blood flow returned completely to normal within 3-4 weeks (consistent with the timeline for neuroadaptation.)25
At the end of the day….
The only completely safe way to approach drugs is not to use them. At least some dosages of MDMA are no doubt neurotoxic in humans, and at this point it’s not clear where the line between neurotoxic and non-neurotoxic doses might be (or even if a clear line can be drawn at all.) Although common recreational doses of MDMA don’t seem to be neurotoxic, it’s important to practice moderation. If you choose to use ecstasy (or any drug), try to carefully limit how often and how much you take. It’s not a matter of all or nothing! Choosing to take one pill doesn’t mean you have nothing more to lose by taking two instead; any increase in use poses increased risks of neurotoxicity and other problems.
For more detailed information and research on MDMA neurotoxicity, visit Erowid.org.
References:
[1] Hatzidimitriou, McCann, and Ricaurte, “Altered serotonin innervation patterns in the forebrain of monkeys treated with MDMA seven years previously: Factors influencing abnormal recovery”, The Journal of Neuroscience, June 15, 1999, 19(12):5096-5107. Abstract.
[2] Scheffel et al., “In Vivo Detection of Short- and Long-Term MDMA Neurotoxicity–A Positron Emission Tomography Study in the Living Baboon Brain”, Synapse 1998, Vol 29:183-192. Abstract.
[3] Reneman et al., “Effects of dose, sex, and long-term abstention from use on toxic effects of MDMA (ecstasy) on brain serotonin neurons”, Lancet, 2001; 358(9296):1864-1869. Abstract.
[4] Buchert et al., “Long-Term Effects of “Ecstasy” Use on Serotonin Transporters of the Brain Investigated by PET”, Journal of Nuclear Medicine 2003; 44:375-384. Abstract.
[5] Rattray, Baldessari, Gobbi, Mennini, Samanin, and Bendotti “p-Chlorophenylalanine Changes Serotonin Transporter mRNA Levels and Expression of the Gene Product” J of Neurochem, 1996; 67(2); 463-472.
[6] Thomasius R, Petersen K, Buchert R, Andresen B, Zapletalova P, Wartberg L, Nebeling B, Schmoldt A “Mood, cognition and serotonin transporter availability in current and former ecstasy (MDMA) users.” Psychopharmacology 2003; 167: 85-96. Abstract.
[7] Sprague and Nichols, “Inhibition of MAO-B protects against MDMA-induced neurotoxicity in the striatum”, Psychopharmacology (Berl), 1995; 118(3):357-359. Abstract.
[8] Yuan et. al., “Effect of depleting vesicular and cytoplasmic dopamine on MDMA neurotoxicity”, Journal of Neurochemistry, Vol 80(6):960-969, 2001. Abstract.
[9] Bai F, Lau SS, Monks TJ “Glutathione and N-acetylcysteine conjugates of alpha-methyldopamine produce serotonergic neurotoxicity: possible role in methylenedioxyamphetamine-mediated neurotoxicity.” Chem Res Toxicol, 1999; 12(12):1150-7. Abstract.
[10] MDMA Neurotoxicity, N. Luno.
[11] Ricaurte, Yuan and McCann, “MDMA (‘Ecstasy’)-Induced Serotonin Neurotoxicity: Studies in Animals”, Neuropsychobiology, 2000; 42(1):5-10. Abstract.
[12] Vollenweider et al., “Effects of MDMA on 5-HT uptake sites using PET and [11C](+)McN-5652 in humans”, Conference of the German Society for Psychiatry, Psychotherapy and Neuromedicine (2000). Abstract.
[13] Malberg JE, Seiden LS “Small changes in ambient temperature cause large changes in 3,4-methylenedioxymethamphetamine (MDMA)-induced serotonin neurotoxicity and core body temperature in the rat” J Neurosci, 1998; 18(13):5086-94. Abstract.
[14] Johnson EA, Shvedova AA, Kisin E, O’Callaghan JP, Kommineni C, Miller DB “d-MDMA during vitamin E deficiency: effects on dopaminergic neurotoxicity and hepatotoxicity” Brain Res, 2002; 933(2):150-163. Abstract.
[15] Schmidt CJ “Neurotoxicity of the psychedelic amphetamine, methylenedioxymethamphetamine” J Pharmacol Exp Ther, 1987; 240(1):1-7. Abstract.
[16] McCann UD, Ricaurte GA “Reinforcing subjective effects of (+/-) 3,4-methylenedioxymethamphetamine (‘ecstasy’) may be separable from its neurotoxic actions: clinical evidence” J Clin Psychopharmacol, 1993; 13(3):214-7. Abstract. (The description listed on this page is the wrong one, but the “Full Text” download link will retrieve the correct file.)
[17] Bolla, McCann, and Ricaurte, “Memory impairment in abstinent MDMA “Ecstasy” users”, Neurology, Vol 51(6):1532-1537, 1998. Abstract.
[18] Simon and Mattick, “The impact of regular ecstasy use on memory function”, Addiction, 2002; 97(12):1523-9. Abstract.
[19] Scheffel U, Lever JR, Stathis M, Ricaurte GA “Repeated administration of MDMA causes transient down-regulation of serotonin 5-HT2 receptors” Neuropharmacology, 1992; 31(9):881-93. Abstract.
[20] Ricaurte GA, Yuan J, Hatzidimitriou G, Cord BJ, McCann UD “Severe Dopaminergic Neurotoxicity in Primates After a Common Recreational Dose Regimen of MDMA (“Ecstasy”)” Science, 2002; 297:2260-2263. Abstract.
[22] Semple et al., “Reduced in vivo binding to the serotonin transporter in the cerebral cortex of MDMA (“ecstasy”) users”, British Journal of Psychiatry, Vol 175, 63-69 (1999). Abstract.
[23] Reneman L, Booij J, Lavalaye J, de Bruin K, Reitsma JB, Gunning B, den Heeten GJ, van Den Brink W “Use of amphetamine by recreational users of ecstasy (MDMA) is associated with reduced striatal dopamine transporter densities: a [123I]beta-CIT SPECT study– preliminary report” Psychopharmacology (Berl) , 2002; 159(3):335-340. Abstract.
[24] Gamma et al., “No Difference in Brain Activation During Cognitive Performance Between Ecstasy (3,4-MDMA) Users and Control Subjects: A [H2 15O]-PET study”, Journal of Clinical Psychopharmacology, Vol 21, No 1 (2001). Abstract.
[25] Chang et al., “Effect of ecstasy (MDMA) on cerebral blood flow: a co-registered SPECT and MRI study”, Psychiatry Research: Neuroimaging Section 98 (2000) 15-28. Abstract.